
WVU Medicine Health System includes 23 hospitals and associated clinics throughout West Virginia. All health system clinics use the EPIC EMR.
Patient population: One third of the population (1.8 million) is covered by Medicaid. West Virginia has some of the highest rates of COPD and Interstitial Lung Disease cases in the United States.
QI Project Team Members and Roles
| QI Team Member | Role |
|---|---|
| Robert Stansbury, MD, ATSF, FAASM | WVU Vaccine Project Lead |
| Nicole Stout, DPT | Vaccine Implementation Science Lead |
| Toni Rudisill, PhD | Vaccine Program Evaluation Lead |
| Jesse Thompson, PhD | Biomedical Research Scientist WVU |
| Kevin Halbritter, MD | Population Health and Data Management Lead |
| Haroon Ahmed, MD | Vaccine Project QI and Clinical Lead |
| Christine Del-Prado Rico, MD | Chief Fellow |
| Sauradeep Sarakar, MD | Senior Fellow |
| Stephanie Boyd, DNP | WVUH Quality Management |
| Hanna Davis | WVUH Quality Analyst |
| Bethany Holt | WVUH Manager Ambulatory Services |
What is one strategy you have tested that has made a difference in improving vaccination rates in your clinic(s)?
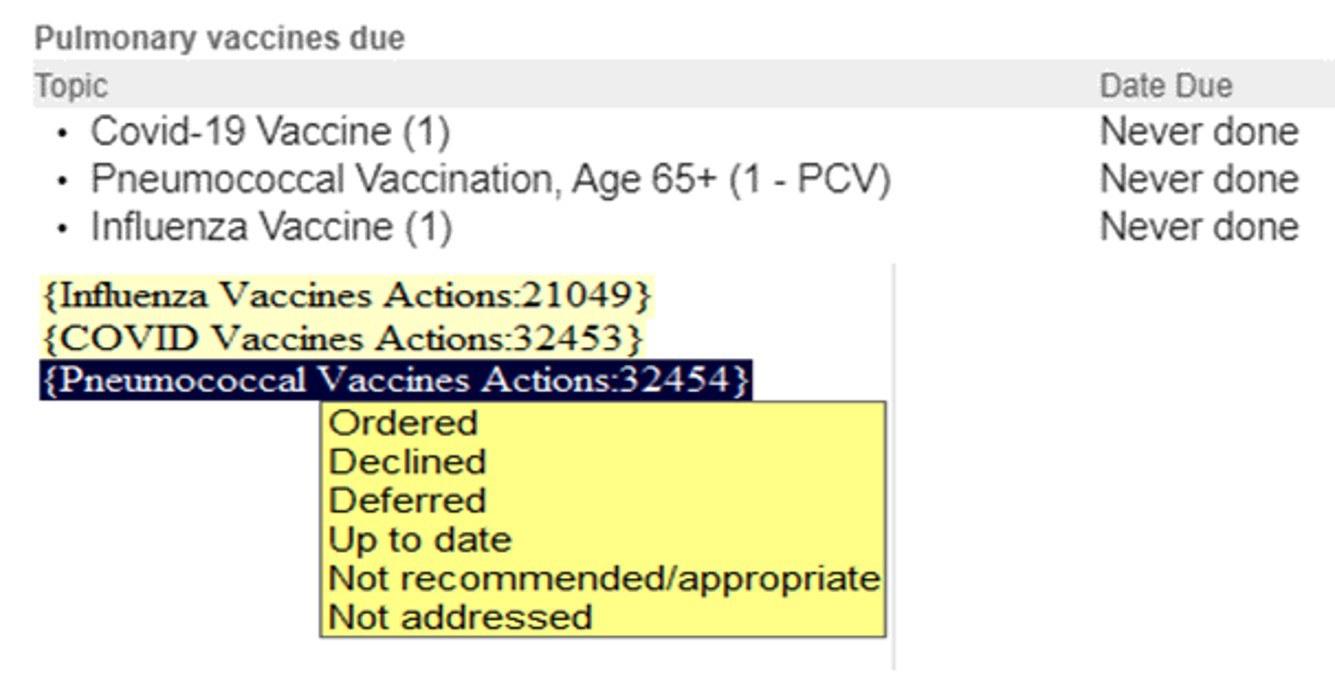
When we initiated the project, it was obvious that we needed a more granular look at the vaccine data to understand what was happening with vaccination in our pulmonary clinics. We developed a dot phrase in the electronic medical record (.pulmvaccine) that could be included in the clinic note. Initially there was poor uptake of this dot phrase. We completed focus groups and structured interviews with pulmonary providers. We received feedback that the vaccine dot phrase did not identify the missing vaccine(s) and added to the burden of completing documentation. We worked with EPIC so the dot phrase would pull in missing vaccines from the health maintenance tab. We iteratively improved that dot phrase responses (below) including a *** that allows providers to put in their own description of the vaccine interaction. The dot phrase can also be embedded in the clinic note template and will be re-activated when bringing a previous note forward for a follow-p visit. Following this iterative improvement uptake of the vaccination dot phrase went from ~10% to about ~70%
Feedback we have received is that this dot phrase serves as a nice reminder for providers to discuss vaccines. We are in the process of reviewing our data for the past year to assess the impact on vaccination rates in our pulmonary clinic, but an early look at our data suggests this simple EMR intervention has led to an increase in vaccination rates.
WVU was one of the vanguard health centers of the ATS Vaccine Initiative and we have found that a number of the health systems coming into the project are following suit with our type of EMR intervention. This intervention provides important data on the clinician-patient interaction, serves as an effective way to assess barriers/facilitators to vaccination, and gives a more granular look at reasons why patient who are due vaccine are not provided with one in clinic.
Based on what you’ve learned, what new strategy will you try in the coming year?
At our recent team meeting we reviewed our clinical workflow diagram (below) that we had developed during our first two team meetings which outlines what needs to occur for a patient to receive a vaccine in our pulmonary clinic. We reviewed the interventions we have initiated and mapped these interventions to FRAME-IS, which is the implementation science framework we utilize for this project. We also reviewed the potential areas for intervention (starred below) that we had not yet developed. Based on this review our team is considering an education intervention targeting patients. This summer we distributed questionnaires to patients following their pulmonary clinic appointment. This questionnaire assessed a communication intervention regarding vaccination that targeted patients. This questionnaire also included general questions to assess thoughts and beliefs on the vaccines of interest. We are currently reviewing this data and hope to develop an effective educational intervention based on this data.

Do you have any patient feedback about their vaccination experience?
After reviewing our patient questionnaire data, we found that many patients prefer to discuss vaccinations directly with a healthcare provider.
Please share a key insight gained from your work to improve vaccination rates.

Our team participated in the ATS Vaccine Initiative learning and sharing session at the ATS 2024 conference. This session brought together representatives from health systems involved in the ATS Vaccine Initiative to share their findings and discuss what they have learned from their work in improving vaccination in clinic. This meeting was phenomenal and I think gave important insights to all those who attended. There were certainly differences between the health systems, but what struck me most were the similarities across the diverse health systems. For instance, most health systems introduced some type of EMR intervention to better identify patients requiring vaccinations. This highlights some universal challenges with current methods of tracking vaccination status such as integration with a state vaccine database or utilizing vaccination status from a health maintenance tab in the EMR. Our team is looking forward to gathering more data on vaccine interventions and further collaboration with the other health systems to identify broad interventions to improve vaccination rates in high risk individuals with respiratory disease. Importantly, we believe our work will identify ways that these interventions can be adapted and tailored to most effectively address vaccination in our local rural communities.