San Francisco Health Network (SFHN) is a publicly funded, vertically integrated urban safety-net of the San Francisco Department of Public Health (SFDPH):
- >100,000 low-income publicly insured, uninsured, undocumented.
- 14 primary care federally qualified health center (FQHC) clinics.
- SFDPH specialty referral services.
- Urban county hospital, rehabilitation hospital, jail health services.
All patients who are part of the SFHN are eligible to receive care at Zuckerberg San Francisco General (ZSFG) hospital campus, which is affiliated with the University of California San Francisco (UCSF).
QI Project Team Members and Roles:

Co-Principal Investigator

Co-Principal Investigator

Project Manager

Immunization Coordinator, Value-Based Care
Kathleen Chung, MD
Medical Director, Value-Based Care
Shibin Tharayil, MPA-HSA
Manager, Value-Based Care
Please share historical context related to vaccine initiatives in San Francisco.
San Francisco has a long and complicated vaccination legacy spanning smallpox outbreaks and the formation of the Anti-Vaccination League in the late 1800s and early 1900s, Chinatown quarantines during the 1900-1904 bubonic plague outbreak, polio vaccination campaigns in the 1950s and 1960s, pronounced distrust and vaccination hesitancy during the HIV/AIDS epidemic, to our vaccine rollout for the COVID-19 pandemic.
What are some of the strategies you have tested that has made a difference in improving vaccination rates in your clinic(s)?
Patients interviewed through focus group work and individual interviews shared that they found their vaccine discussions with our staff unsatisfactory. These interactions were described as rushed, inconsistent, and superficial. Staff from multiple clinics shared that they did not feel confident having complex counseling conversations citing time pressure, reluctance to engage with patients who express vaccine hesitancy, and lack of discussion tools as principal barriers.
Vaccine hesitancy training
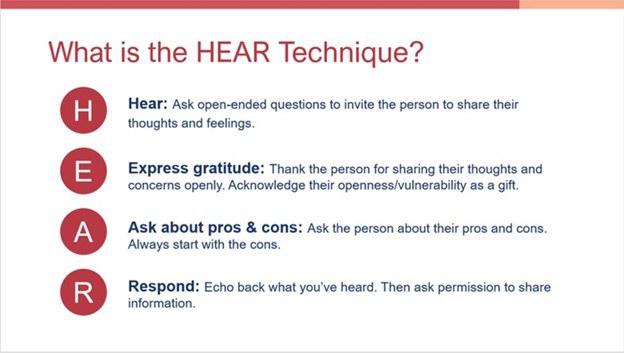
We developed a technique called “HEAR” training to teach clinic staff and providers how to engage respectfully with patients who are hesitant about vaccines. HEAR is an acronym for Hear, Express Gratitude, Ask Pros and Cons and Respond (Figures 1 and 2). HEAR trainings are interactive, featuring scenario presentation and practice, and are tailored to serviced patient populations.
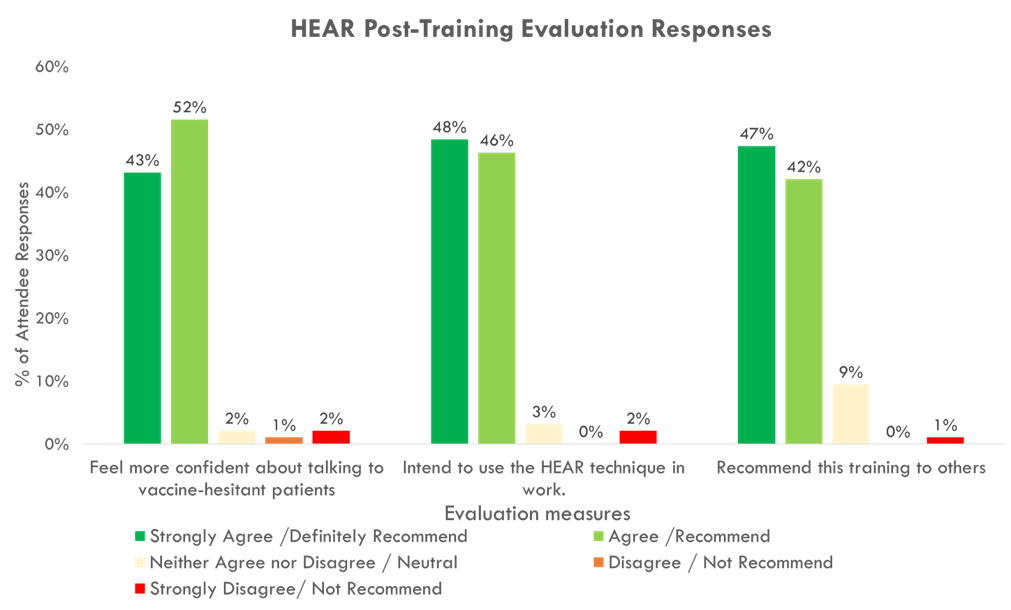
In Fall 2023, we held eight 30-minute trainings for over 125 clinical staff in preparation for influenza season 2023-2024. Post-training evaluations showed high rates of staff feeling more confident about engaging with vaccine-hesitant patients and high rates of intent to use the HEAR technique in practice (Figure 3).
System-wide, 49% of pulmonary patients across our system received an influenza vaccination in the 2023-2024 influenza season, compared to 40% in the 2022-2023 influenza season. Causal attribution of this increase in influenza vaccination rates to HEAR training is difficult to establish. However, we expect our broad-based HEAR training to help standardize our system-wide approach to engaging patients in vaccination discussions and, over time, raise our patient expectations to experience a culture of respectful engagement around vaccines. We also postulate that a positive “priming” environment will be established with each touch point increasing the likelihood of eventual vaccine acceptance and receipt.
More information about the HEAR technique can be found on the UCSF Center for Excellence in Primary Care website.
Pop-up influenza vaccine clinic
Our pop-up vaccination clinic was designed to be a small footprint, easy-to-set-up, accessible vaccination resource. The clinic is located in the main ambulatory care lobby at Zuckerberg San Francisco General (ZSFG) hospital and is staffed by two nurses who speak English, Spanish, and Cantonese – the top 3 languages spoken by our patient population. Upon entering the hospital lobby, patients are greeted by nurses and asked if they are interested in influenza vaccination.


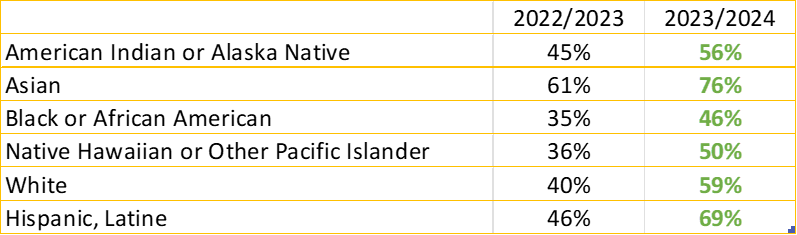
When HEAR technique was accompanied by influenza vaccine champions, distribution of language concordant flyers, and a walk-in Urgent Care influenza vaccine pop-up clinic, we saw an overall influenza vaccination rate in the Urgent Care Clinic of 60.5% and increases in vaccination rates across all racial groups (2023-2024) compared to last year’s influenza season (2022-2023) (Table 1).
Based on what you’ve learned, what new strategy/strategies will you try for the in the coming year?
Influenza vaccination rates from the 2023-2024 season for patients with chronic lung disease showed an early “sprint zone” (October-November) where 81% of those patients that ultimately received the influenza vaccine were vaccinated, a “fatigue zone” (December-January) showing a steep drop-off in offer rates and vaccinations accounting for 15% of all patients vaccinated, and a “refractory zone” (February-April) accounting for only 4% of all patients vaccinated. Furthermore, only 15% of patients with chronic lung disease received their influenza vaccine in a pulmonary specialty clinic, whereas 30% received their influenza vaccine in a primary care setting.
For the 2024-2025 flu season, we’re implementing the following changes:
- HEAR training starting in September 2024 (compared to October 2023).
- Broad dissemination of HEAR training to primary care and specialty care clinic personnel.
- Refresher training before December in anticipation of staff “fatigue” to maintain high offer rates.
- Front-loaded resources to capture most patients during the early season. The influenza pop-up clinic was opened in mid-September 2024 (compared to October 2023).
Do you have any patient feedback about their vaccination experience?
“I notice that the clinic (personnel) seems more patient with me this year when I say I’m still thinking about getting the vaccine…” (patient from primary care clinic ZSFG)
“They listen more and are less pushy. I appreciate that.” (patient from Chest Clinic ZSFG)
Please share a key insight gained from your work to improve vaccination rates.
System-wide changes are required to make the largest impact on vaccination rates in the SFHN. Working directly with our Department of Value-Based Care has been critical to achieving the necessary buy-in from executive sponsors and operational stakeholders to move initiatives forward.