Measles, also known as rubeola, is a disease caused by the measles virus.
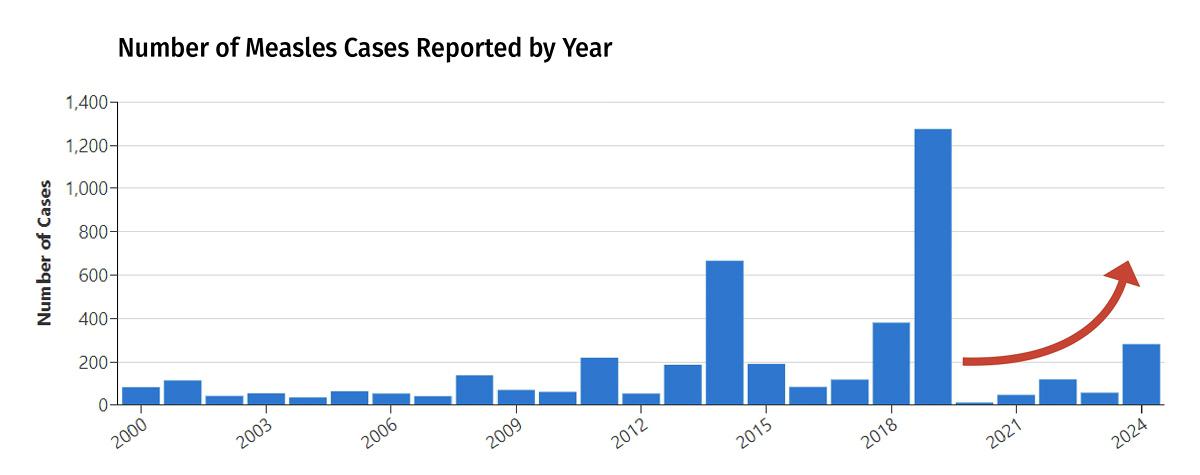
Before routine measles vaccination began in 1963, nearly everyone got infected with measles during childhood. Once the measles vaccine became widespread, the number of measles cases dropped to fewer than 150 cases per year from 2001 to 2010. Since 2012, the number of U.S. measles cases has ranged between 13 to 1274 annually. The peak incidence (1274 cases) was observed in 2019. In 2024, 283 cases of measles have been reported, including 16 outbreaks (defined as >2 cases), and 70% (198/283) of measles infections were outbreak-associated. In contrast, 4 outbreaks were reported in 2023 and 49% (29/59) were outbreak-associated. This is a major public health concern because of how easily the virus spreads and how serious the infection can be.
How is measles spread?
Measles is spread from person-to-person. The virus enters your body through the eyes, nose, or mouth. You can get sick by being exposed to an infected person who is coughing, sneezing, or from secretions on their hands. The virus can also live up to 2 hours on surfaces and in contaminated air spaces. Measles is highly contagious: up to 90% of people who have not had vaccine and who come in close contact with an infected person will develop the disease. In comparison, only about 25% of the people living in the same home as a person with influenza will contract the flu themselves. Measles can cause outbreaks in areas where vaccination rates are less than 95% and outbreaks are occurring worldwide. Symptoms start within 7–14 days of exposure.
What are the symptoms of measles?
The symptoms of measles resemble that of the flu, along with a rash. The disease generally starts with a high fever, cough, runny nose, and red, watery eyes. In 2–3 days, white spots may appear on the inside of the mouth, known as Koplik spots (below). After 3–5 days, a rash consisting of small red spots and bumps (above) appears first on the face and head and then spreads to the rest of the body. People who have measles are thought to be contagious from 4 days before the rash appears until 4 days after. Measles symptoms typically resolve within 1–2 weeks.
How is measles diagnosed?
Measles is diagnosed based on the presence of flu-like symptoms, a rash that spreads from head-to-toe, and mouth lesions. However, many healthcare providers have not seen measles cases and may not readily recognize the disease. Measles can be confirmed by testing for the virus with a throat swab.
Is measles dangerous?
Up to 40% of people who get measles will have other health problems (complications) from the infection. The most common complications are ear infection and diarrhea, which occur in about 10% of infected children. Pneumonia occurs in about 5% of infected children. Measles can cause inflammation of the brain (encephalitis) in 1 of every 1000 infections and more rarely may cause blindness. About 1–3 children out of every 1000 infected will die from respiratory and neurologic complications from measles. Adults over the age of 20 years tend to have more severe symptoms and are more likely to need hospitalization. A person who has measles is also more at risk (susceptible) for other infections so they may get a new bacterial infection as well. People who have weakened immune systems, very young infants, and pregnant women are at higher risk of having a serious measles infection.
How is measles treated?
There is no specific treatment for measles. Antibiotics are not helpful as this is a viral infection and not a bacterial infection. Vitamin A may reduce complications and is recommended for all children with measles. An antiviral medication that targets the measles virus is currently being developed, though it has not yet been tested in humans.
How is measles prevented?
Vaccination against measles is more than 97% effective in preventing the disease. Two doses are recommended: the first at 12–15 months of age, and a second dose at 4–6 years of age. The vaccine can also be given to people who have not had the vaccine within 72 hours of an exposure to the virus to help prevent infection. People with poor immune system function and those at risk of severe complications, such as infants < 1 year old and pregnant women who were not vaccinated, should be given immunoglobulin (concentrated antibodies derived from the plasma of blood donors) after measles exposure to reduce the risk of infection. Vaccination and natural infection both provide lifelong immunity. People born before 1957 are presumed to have had the disease and have immunity.
Is the measles vaccination safe?
The measles vaccine is extremely safe. It is typically given in combination with vaccines against mumps and rubella, known as the MMR vaccine. The measles vaccine is composed of a live, weakened strain of the virus, which allows the body to develop antibodies that will be protective when exposed to the actual measles virus. The most common side effects of the MMR vaccine are soreness at the injection site, fever, mild rash, and joint pain or stiffness. Febrile seizures occur in about one in 3,000 to 4,000 children receiving the vaccine (compared to one in 1,000 children who have seizures with fever while sick with measles). Febrile seizures can be frightening but are almost always self-limited and resolve without complications. A link between the MMR vaccine and autism was proposed in the 1990s based on falsified information and fraud and was since disproved. It is important that all people who can be vaccinated receive the vaccine. This benefits the person and helps protect those who cannot receive the vaccine due to a serious allergy or weakened immune system. This is known as “herd immunity.”
Why is the rate of measles infection increasing?
There are many areas of the world where vaccine coverage is insufficient to provide herd immunity. Many regions in the U.S. now have vaccine rates below 90%. Globally, first-dose measles vaccine coverage has been steady at 85%, and second-dose coverage is 67%. Worldwide, outbreaks are increasing. In the U.S., most outbreaks are related to people who have not had vaccine traveling abroad and getting infected with measles (importation). Recently importations have come from the Philippines, Ukraine, Israel, Thailand, Vietnam, England, France, Germany, and India. Travelers bring the infection back to the U.S. and it spreads quickly in communities at home with low vaccination rate.
Getting Vaccinated
The most important protective measure against measles is vaccination. If vaccination records are not available and vaccination status is unknown, then vaccination with MMR is recommended. There is no harm in receiving another vaccine dose if a person has already received it in the past. A booster is not recommended for people who have already received two doses of the vaccine. A booster dose is advised for those who have received only one dose. Measles is more common in certain countries, and the CDC Travel Notices provide information on measles exposure risk (https://www.cdc.gov/measles/travel/index.html). If you think you have been exposed to measles and were not vaccinated, contact a healthcare provider right away to get a vaccine.
-----
Authors: Jane E. Gross MD, Jonathan M Keller, MD; Charles S. Dela Cruz MD, PhD; Susan Pasnick MD;, PhD; W. Graham Carlos MD; Ryan Maves, MD; Shazia Jamil, MD on behalf of the ATS Late Breaking Learning Committee.
Reviewers: Marianna Sockrider, MD, DrPH
Topper image source: Centers for Disease Control and Prevention American Thoracic Society.
Graph source: Centers for Disease Control and Prevention (trend indicator arrow added).
-----
References & Sources
Melegaro A. Measles vaccination: no time to rest. Lancet Glob Heal. 2019;7(3):e282-e283. doi:10.1016/S2214-109X(18)30531-X
World Health Organization - MMR and Autism
Centers for Disease Control and Prevention
American Academy of Pediatrics—Healthy Children.org
Shot by Shot.org—stories of vaccine-preventable diseases
PUBLIC HEALTH SERIES
ATS Patient Education Series © 2025 American Thoracic Society | Online version updated January 2025