Author
Fahid Alghanim, MD, Pulmonary and Critical Care Fellow, Department of Internal Medicine, Division of Pulmonary and Critical Care, University
of Maryland School of Medicine
Ellen Marciniak, MD, Assistant Professor, Department of Internal
Medicine, Division of Pulmonary and Critical Care, University of
Maryland School of Medicine
Case
A 59-year-old man with a history of COPD and unresectable stage IIIA Squamous Cell Carcinoma of his Right lower Lobe (RLL) in 2012 treated with concurrent chemo- and radiation therapy who had pathologically proven local recurrence of disease in 2018 which was treated with combined chemotherapy (Carboplatin & Abraxane) and Immune Modulate Proton Therapy (IMPT) (6120 cGy) presented with 2 weeks of progressively worsening dyspnea and pleuritic chest pain.
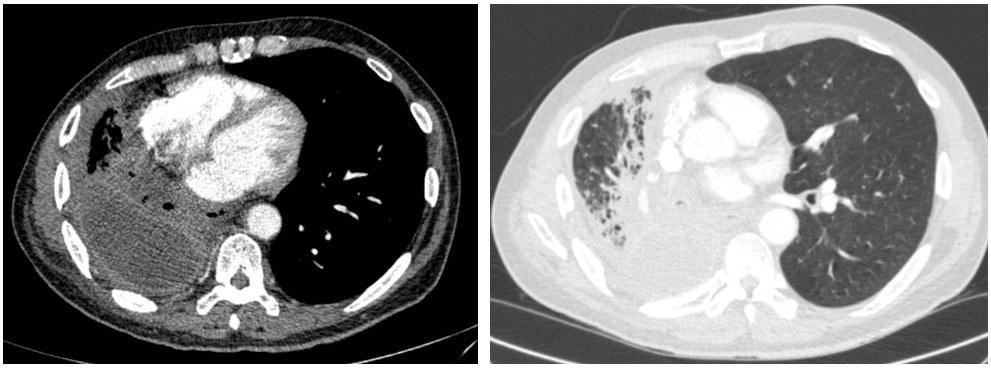
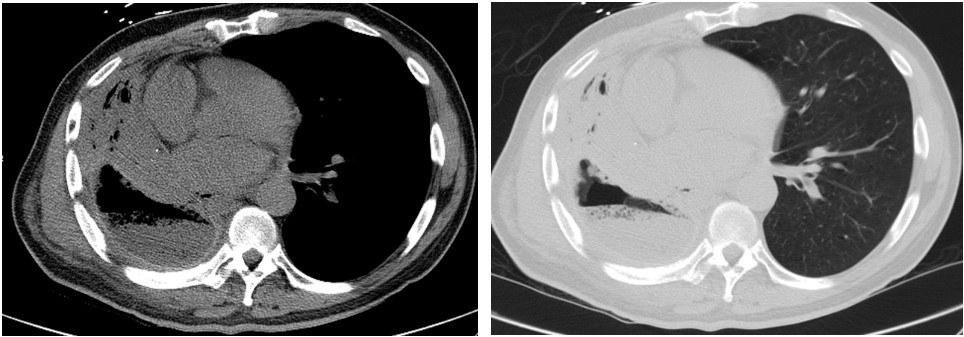
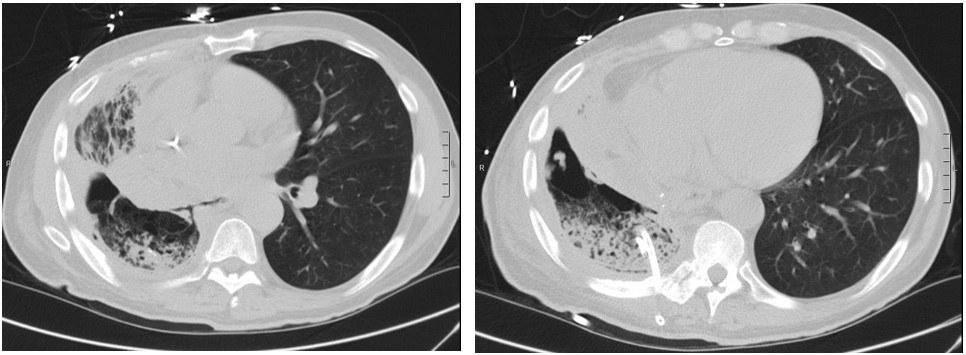
On evaluation, he was tachycardic with fever (38.6 °C) and exhibited decreased air entry to his RLL. Contrast enhanced Computed Tomography (CT) of the chest was done and showed right middle and lower lobe consolidation with areas of cavitation and a moderate right sided pleural effusion (Image 1). The patient was started on broad spectrum antibiotics. A repeat CT chest was obtained on day 7 due to clinical deterioration, which showed a new right-sided hydropneumothorax (Image 2). A pigtail chest tube was placed by Interventional Radiology that drained brown, markedly turbid fluid that was exudative based on Light’s criteria (pH < 6.3, LDH 575). His chest tube output continued to drain copious volume (average: 400 ml/day) of turbid, foul-smelling fluid with particulate matter over the next few days. Microbiological data identified polymicrobial growth of oral/upper respiratory tract: GPC in pairs and chains, GPRs, and candida glabrata. Subsequent CT chest after chest tube placement is shown below (Image 3):
Question
What is the most likely cause of his clinical symptoms?
A. Bronchopleural Fistula
B. Esophageal pleural fistula
C. Lung Abscess
D. Iatrogenic Hydropneumothorax
