Authors
Harshkumar Patel, MBBS 1; Christian Woods, MD 2
1Department of Medicine, MedStar Washington Hospital Center, Washington, DC
2Department of Medicine, Sections of Infectious Diseases and Pulmonary/Critical Care Medicine, MedStar Washington Hospital Center, Washington, DC
Case
A 66-year-old male presented with a 5-day history of progressive shortness of breath, right sided pleurisy, and productive cough. Associated symptoms included night sweats and malaise, but he denied fevers, chills, or hemoptysis. His medical history was significant for emphysema, opioid use disorder, untreated hepatitis C infection, and diabetes mellitus. His home medications included methadone and albuterol as needed. He was an active tobacco smoker having smoked 1 pack of cigarettes per day since his early 20s. He denies sick contacts, recent travel, or significant occupational exposures.
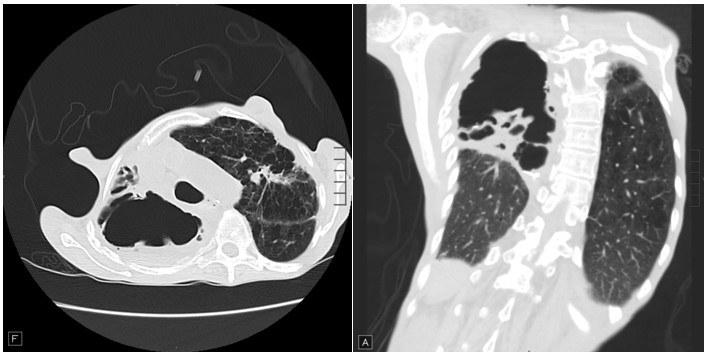
On exam, he was afebrile but tachycardic with heart rate of 105 beats/minute and tachypneic with respiratory rate of 22 breaths/minute. He was not in any significant distress. His lung exam was significant for decreased breath sounds in all lung fields with prominent hyperresonance in right upper lung fields. He had finger clubbing and evidence of fat and muscle wasting. Chest X-ray shows air fluid levels in right upper lung spaces. Sputum cultures were obtained. Images from his high-resolution CT scan of Chest are shown below:
Question
In addition to antibiotics, what is the next best step in management?
A. Bronchoscopy with bronchoalveolar lavage
B. CT or fluoroscopy guided aspiration
C. Expectant management
D. Tube thoracostomy