Authors
Avraham Z. Cooper, MD1, Jennifer W. McCallister, MD2, and Namita Sood, MD3.
1Pulmonary/Critical Care Medicine Fellow, Division of
Pulmonary, Critical Care & Sleep Medicine, Ohio State University
Wexner Medical Center, Columbus, OH.
2Associate Clinical Professor in the Division of
Pulmonary, Critical Care, & Sleep Medicine and Program Director of
the Pulmonary & Critical Care Medicine Fellowship, Ohio State
University Wexner Medical Center, Columbus, OH.
3Professor of Critical Care, Pulmonary & Sleep
Medicine and Director of the Pulmonary Vascular Disease Program,
University of Texas, McGovern Medical School, Houston, TX.
Case
A 25-year-old woman without significant past medical history
presented with three weeks of progressive dyspnea, productive cough,
fevers, generalized fatigue, and malaise. She lived in a rural area in
the Midwest and was a non-smoker. She denied weight loss, night-sweats,
rash, or joint pain or swelling. Three weeks prior to presentation she
was exposed to a large amount of dust during the Fall harvest on a
vegetable farm. She did not have any other exposures. Chest examination
revealed bilateral inspiratory rhonchi. Labs were notable for mild
transaminitis, an elevated C-reactive protein to 108 mg/L, with normal
complete blood count and serum chemistry panels, as well as negative
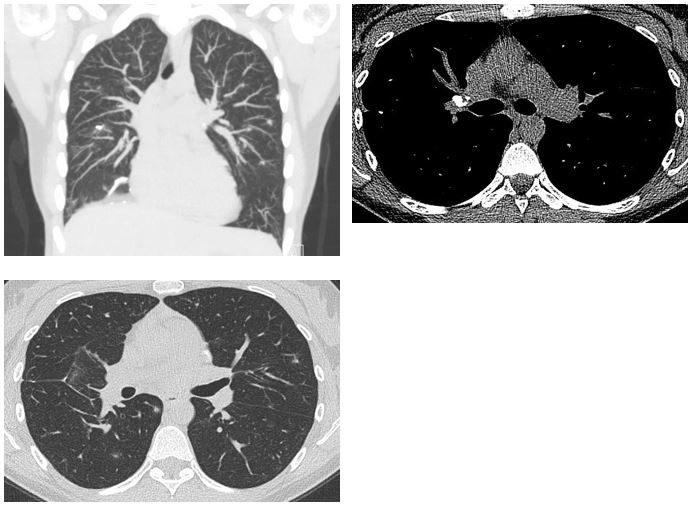
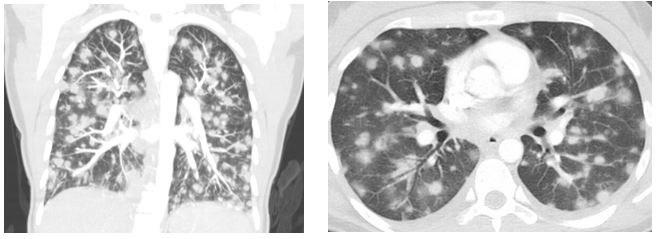
antinuclear cytoplasmic antibodies (ANCA). Representative CT scan images
of the chest are shown below (Figure 1).
Figure 1
Question
What is the most likely diagnosis?
A. Metastatic malignancy
B. Pulmonary vasculitis
C. Severe fungal infection