Author
Janaki Deepak, MBBS, FACP
Assistant Professor, Pulmonary and Critical Care Medicine,
University Of Maryland School Of Medicine, Baltimore, MD
Case
A 57 year old male with hypertension and hyperlipidemia presented with vague discomfort in the chest, shortness of breath and malaise for a few weeks. He denied any cough, fever, orthopnea, or palpitations. He has had decreased appetite and 5 pound weight loss.
Social History: Smoker, 40 pack year smoking history. Denies alcohol or drug use. Some exposure to asbestos in his early 20s.
Physical exam: T: 36.5, P: 98, BP: 110/67, RR: 20, 95% on room air
General: Obese male in minimal distress. Lungs: Decreased breath sounds on the left upper zone, no egophony, no dullness to percussion.
Heart: S1, S2 normal no murmurs, rubs, gallop
Basic labs and EKG are normal.
Chest x-ray
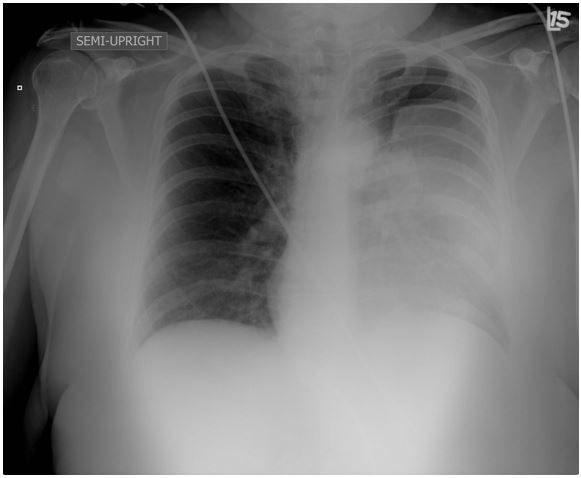
Question
Based on the Chest x-ray above what would be the next best step in management of this patient?
- Admit the patient and start on antibiotics for community acquired pneumonia
- Perform an ultrasound guided thoracentesis
- Obtain a CT and plan for a bronchoscopy for tissue biopsy
- Inform the patient that his x-ray only shows an artifact (skin fold mimicking haziness) and discharge home.

