Authors
Robert A. Case, M.D.1, Catherine Gonsalves, M.D.3, Simon Ho, M.D.4, Brian Stewart, M.D.3 Divya C. Patel, D.O.2, Diana C. Gomez-Manjarres, M.D.2
1Department of Medicine; University of Florida
2Division of Pulmonary, Critical Care, and Sleep Medicine; University of Florida
3Department of Pathology, Immunology and Laboratory Medicine; University of Florida
4Department of Diagnostic Radiology; University of Florida
Case
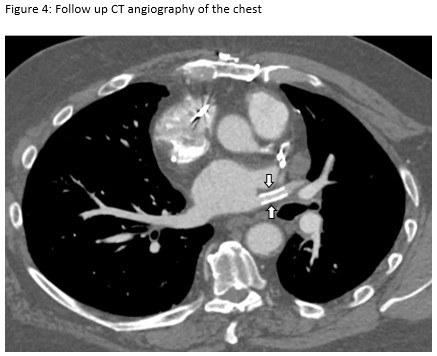
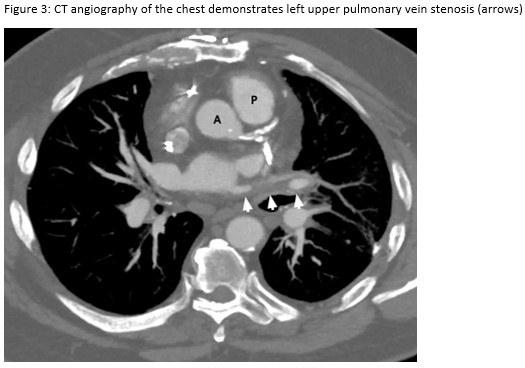
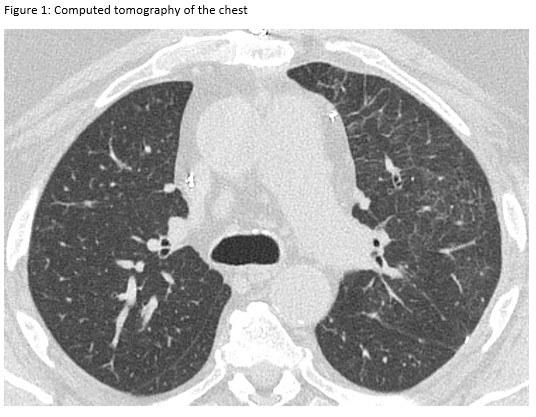
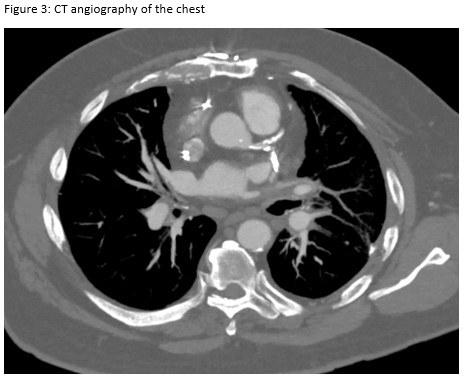
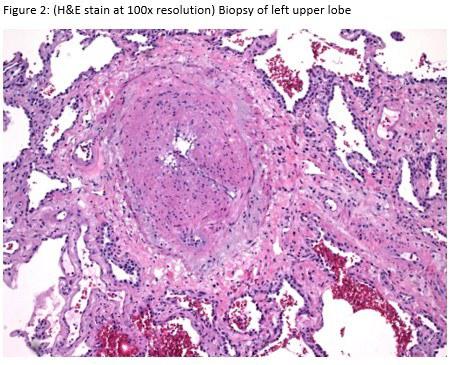
A 72-year-old man presented for evaluation of progressive dyspnea with concern for interstitial lung disease (ILD). He had an extensive cardiac history with prior cardiac bypass surgery and atrial appendage exclusion, followed by multiple subsequent radiofrequency ablations targeting arrhythmogenic foci. His last ablation procedure was three years prior to presentation. He reported reduced exertional tolerance, and was only able to ambulate a few blocks. As a part of his work-up, his local pulmonologist had obtained a high-resolution computed tomography (HRCT) of the chest, which showed abnormalities limited to the left upper lobe (Figure 1). He was treated with antibiotic therapy and corticosteroids but had no improvement so a surgical lung biopsy was performed. These images and biopsies were reviewed at our institution. A representative picture of histology from the biopsy is shown in Figure 2. After his visit to the ILD clinic, a CT angiogram of the chest was obtained and is shown in Figure 3.
Question
What is the most likely diagnosis based on this information?
A. Interstitial lung disease
B. Pulmonary embolism
C. Adenocarcinoma in situ
D. Pulmonary vein stenosis
E. Atypical pneumonia