Authors: A Chapa-Rodriguez MD1, C O’Rear DO1, P. Gopinath MD1, Y Medina MD2
1 - Department of Pulmonary and Critical Care
2 - Department of Neurology
Case
61 y/of with PMH Essential Hypertension, COPD, recurrent pneumonia, chronic pain syndrome, anxiety, migraine. Presented to the ED after mechanical fall. Found to be hypoxic. Diagnosed with pneumonia. Hospitalization has been characterized by progressive decline and generalized weakness being unable to lift a cup of water or reposition in bed. Symptoms started 3 months prior to admit with LE weakness being more pronounced. She has had multiple therapeutic bronchoscopies for mucus plugs owing to difficulty coughing up her secretions secondary to weak cough.
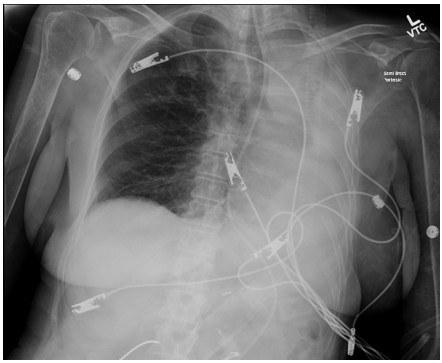
MRI Brain and c spine without acute abnormalities, b12, HIV and TSH within normal limits. Chest X Ray shows left lung atelectasis with ipsilateral mediastinal shift.
Physical exam showed diffuse symmetric weakness, more pronounced in the lower extremities, absent Achilles reflexes, hyperreflexia at the knees, and bilateral Babinski signs. Sensation is intact. Extraocular movements and facial strength preserved.

Correct!
Discussion
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder characterized by both upper (UMN) and lower motor neuron (LMN) involvement. It manifests clinically as muscle weakness, atrophy, fasciculations, hyperreflexia, spasticity and a positive Babinski sign. Typically presenting in mid-to-late adulthood, the initial weakness is often asymmetric and focal (such as hand clumsiness or foot drop) before spreading regionally. Bulbar involvement is seen in 25–30% of cases leading to dysarthria or dysphagia. Diagnosis pivots in demonstrating the presence of both UMN and LMN signs across multiple regions, supported by EMG findings of widespread denervation and reinnervation, alongside neuroimaging and lab tests that exclude alternative explanations. This leads to an average time to diagnosis of 13–18 months.
ALS mimickers may share ALS-like-features, however there are key distinctions that help differentiating them from ALS. For example, primary lateral sclerosis (PLS) exhibits purely UMN involvement (no muscle wasting or fasciculations) and it progresses more slowly; EMG lacks denervation findings seen in ALS. Progressive muscular atrophy (PMA) demonstrates only LMN signs and may remain confined to lower motor neuron dysfunction for months to years without UMN involvement. Multifocal motor neuropathy, myasthenia gravis, inclusion body myositis, Eaton–Lambert syndrome, AIDP and CIDP are differentiated clinically and via specific diagnostic test. See table below.
ALS vs. Mimickers: Comparison Table
| Condition | Similarities to ALS | Distinguishing Features | Diagnostic Clues / Tests |
|---|---|---|---|
| ALS | Progressive asymmetric motor weakness (insidious onset, months to years) UMN + LMN signs No sensory involvement | No bowel/bladder/sensory symptoms Progressive, fatal course Normal imaging Fasciculation and bulbar symptoms , | EMG: widespread denervation MRI: often normal Clinical diagnosis (El Escorial criteria) |
| Cervical Spondylotic Myelopathy | UMN signs in legs LMN signs in arms Weakness | Sensory level often present Spastic gait May have radicular pain | MRI: spinal cord compression EMG: radiculopathy pattern |
| Multifocal Motor Neuropathy (MMN) | Progressive asymmetric distal weakness LMN signs | No UMN signs Responds to IVIG Often younger onset | EMG: conduction block Anti-GM1 antibodies often positive |
| Primary Lateral Sclerosis (PLS) | Progressive spasticity UMN signs only | No LMN signs Much slower progression Better prognosis | EMG: no denervation Diagnosis of exclusion |
| Spinal Muscular Atrophy (Adult-onset) | LMN weakness Atrophy, fasciculations | No UMN signs Often familial Earlier onset | Genetic testing (SMN1 deletion) EMG: denervation without UMN |
| Inclusion Body Myositis (IBM) | Progressive muscle weakness Asymmetric involvement | Involves finger flexors and quadriceps No UMN signs May have mild CK elevation | Muscle biopsy: rimmed vacuoles EMG: myopathic changes |
| Myasthenia Gravis | Weakness, dysphagia, dysarthria | Fluctuating weakness No UMN/LMN signs Extraocular involvement | AChR or MuSK antibodies Positive edrophonium test EMG: decrement on repetitive stimulation |
| Eaton-Lambert Syndrome (LEMS) | Proximal weakness Bulbar and respiratory involvement in severe cases | Autonomic symptoms (dry mouth, impotence) Improves with activity (facilitation) Hyporeflexia improves after exercise | EMG: incremental response with rapid stimulation Anti-VGCC antibodies Associated with small cell lung cancer |
| Bulbar Palsy (Isolated) | Dysarthria, dysphagia Tongue atrophy | No limb involvement No UMN signs | MRI/CT: rule out structural causes EMG: localized denervation |
| Paraneoplastic Motor Neuron Syndromes | ALS-like presentation Subacute progression | Often associated with other symptoms (e.g., weight loss) Rapid decline | Onconeural antibodies (e.g., anti-Hu) Search for malignancy |
| Heavy Metal Toxicity (e.g., Lead) | LMN signs Weakness | Associated GI/renal symptoms May have encephalopathy | Blood/urine heavy metal levels |
| Hexosaminidase A Deficiency (Adult Tay-Sachs) | LMN weakness Fasciculations | Often Jewish descent May have psychiatric symptoms | Enzyme assay Genetic testing |
| AIDP | LMN, progressive Muscle weakness, | LMN only, sensory involvement, reflex markedly reduced or absent, fasciculations and bulbar involvement are rare | rapid progression, ascending weakness, often post infectious EMG – demyelination ( no reinnervation ) |
| CIDP | LMN Muscle weakness over weeks to months | LMN only, sensory involvement, reflex markedly reduced or absent, fasciculations and bulbar involvement are rare | Slow progressive or relapsing-remitting symmetric proximal and distal EMG – demyelination and conduction block ( no reinnervation ) |
References
- Wijesekera LC, Leigh PN. Amyotrophic lateral sclerosis. Orphanet J Rare Dis. 2009;4:3.
- Turner MR, et al. Mimics and chameleons in motor neurone disease. Pract Neurol. 2013;13(3):153–164.
- Dalakas MC. Advances in the diagnosis, pathogenesis and treatment of CIDP. Nat Rev Neurol. 2011;7(9):507–517.
- van Doorn PA, et al. Diagnosis, treatment and prognosis of Guillain-Barré syndrome (AIDP). Nat Rev Neurol. 2008;4(9):442–453.
- Léger JM, et al. Chronic inflammatory demyelinating polyradiculoneuropathy: from pathology to phenotype. J Neurol Neurosurg Psychiatry. 2018;89(12):1261–1272.
- Dimachkie MM, Barohn RJ. Multifocal motor neuropathy. Neurol Clin. 2013;31(2):533–550.
- Sharma KR, et al. Electrodiagnostic criteria for motor neuron diseases. Muscle Nerve. 2008;37(4):498–506.
- Statland JM, Barohn RJ, Dimachkie MM. Muscle disease mimics of ALS. Continuum (Minneap Minn). 2015;21(5):1422–1444.
Not quite.